
Can a Vegan Diet Help With Autoimmune Disease Symptoms? Understanding the Science Behind Plant-Based Eating and Inflammation

Living with an autoimmune disease often means navigating a complex relationship with food and inflammation. As more people explore dietary approaches to managing their symptoms, plant-based eating has garnered increasing attention. Let’s explore what the research tells us about the potential benefits and considerations of a vegan diet for autoimmune conditions.
The Inflammation Connection
Autoimmune diseases are characterized by the immune system mistakenly attacking healthy cells, leading to chronic inflammation. What we eat can significantly impact inflammation levels in our bodies. Plant-based diets are naturally rich in anti-inflammatory compounds like antioxidants, polyphenols, and fiber, which may help reduce systemic inflammation.
What the Research Shows
Several studies have shown promising results regarding plant-based diets and autoimmune conditions. For example, research has found that people with rheumatoid arthritis often report reduced joint pain and improved mobility when following a vegan diet. Similarly, some studies suggest that plant-based eating may help manage symptoms of multiple sclerosis, lupus, and other autoimmune conditions.
Key Benefits of a Vegan Diet for Autoimmune Conditions
- Increased Fiber Intake
Fiber feeds beneficial gut bacteria, which play a crucial role in immune system regulation. A healthy gut microbiome may help reduce inflammation and improve autoimmune symptoms. - Elimination of Common Trigger Foods
Many animal products contain compounds that can trigger inflammation in sensitive individuals. A vegan diet naturally eliminates dairy, eggs, and meat products that some people with autoimmune conditions find problematic. - Higher Antioxidant Content
Plant foods are rich in antioxidants that help combat oxidative stress and inflammation. Foods like berries, leafy greens, and colorful vegetables provide particularly high levels of these protective compounds.
Important Considerations
While a vegan diet shows promise for managing autoimmune symptoms, it’s essential to approach any dietary change thoughtfully:
Nutrient Adequacy
Those with autoimmune conditions must ensure they’re getting adequate nutrients, particularly vitamin B12, iron, zinc, and vitamin D. These nutrients can be obtained through fortified foods or supplements on a vegan diet.
Individual Variation
Not everyone responds the same way to dietary changes. Some people with autoimmune conditions may find that certain plant foods, such as nightshades or legumes, trigger their symptoms.
Quality Matters
A whole-food, plant-based approach focusing on minimally processed foods is likely to be more beneficial than a vegan diet heavy in processed alternatives.
Practical Implementation
If you’re considering trying a vegan diet to help manage autoimmune symptoms, consider these steps:
- Consult Healthcare Providers
Work with your healthcare team to ensure a vegan diet is appropriate for your specific condition and circumstances. - Start Gradually
Consider transitioning slowly to allow your body to adjust and to better identify which changes impact your symptoms. - Keep a Symptom Journal
Track your symptoms, energy levels, and any changes you notice as you modify your diet. - Focus on Nutrient-Dense Foods
Include a variety of colorful vegetables, fruits, whole grains, legumes, nuts, and seeds to ensure comprehensive nutrition.
Additional Lifestyle Factors
Remember that diet is just one piece of the puzzle. Managing autoimmune conditions typically requires a comprehensive approach that includes:
- Adequate sleep
- Stress management
- Regular gentle exercise
- Proper medication management
- Social support
The Bottom Line
While a vegan diet shows promise for helping manage autoimmune symptoms, it’s not a cure-all or guaranteed solution for everyone. The relationship between diet and autoimmune disease is complex and highly individual. Some people may find significant relief from symptoms on a plant-based diet, while others might need different approaches.
If you’re interested in exploring how a vegan diet might help with your autoimmune condition, work with healthcare providers who can help you make informed decisions and ensure your nutritional needs are met. They can help you develop a personalized approach that takes into account your specific condition, symptoms, and overall health goals.
Remember that managing an autoimmune condition is a journey, and dietary changes are just one tool in your toolkit. Be patient with yourself as you explore what works best for your body, and stay open to adjusting your approach as needed.
According to Hunnes, anti-inflammatory vegan foods that could help manage autoimmune flare-ups include:

1) Whole grains
Whole grains are what you get when all three layers of the kernel—bran, endosperm, and germ—have been left intact. Whole grains are a good source of complex carbohydrates, fiber, protein, iron, B vitamins, antioxidants, polyphenols, and other minerals.
Refined grains, on the other hand, have been stripped down to just the endosperm, removing most of the nutrients. This is why so many white bread and pasta products are enriched with added vitamins and minerals.
It’s especially common for people with autoimmune diseases to go gluten-free. In this case, you should avoid whole wheat, rye, barley, farro, spelt, freekeh, wheat berries, and couscous, which is made from durum wheat.
Gluten-free whole grains include brown rice (hello, vegetable fried rice with tofu!), oats, buckwheat, quinoa, sorghum, and millet. Most supermarkets carry pasta, bread, and cereal made from gluten-free whole grains.
 Canva
Canva
2) Nuts and seeds
Many nuts and seeds contain flavonoids, antioxidants like vitamin E, and other plant compounds that help fight inflammation. They also contain heart-healthy unsaturated fatty acids, including omega-3, which research suggests can protect from inflammation as well.
Add a wide variety of nuts and seeds to your diet, such as walnuts, almonds, chia seeds, flaxseeds, pistachios, and pecans. A small handful of nuts or seeds is roughly a serving and can make a good snack. Nut butter is a great mix-in for oatmeal and smoothies.
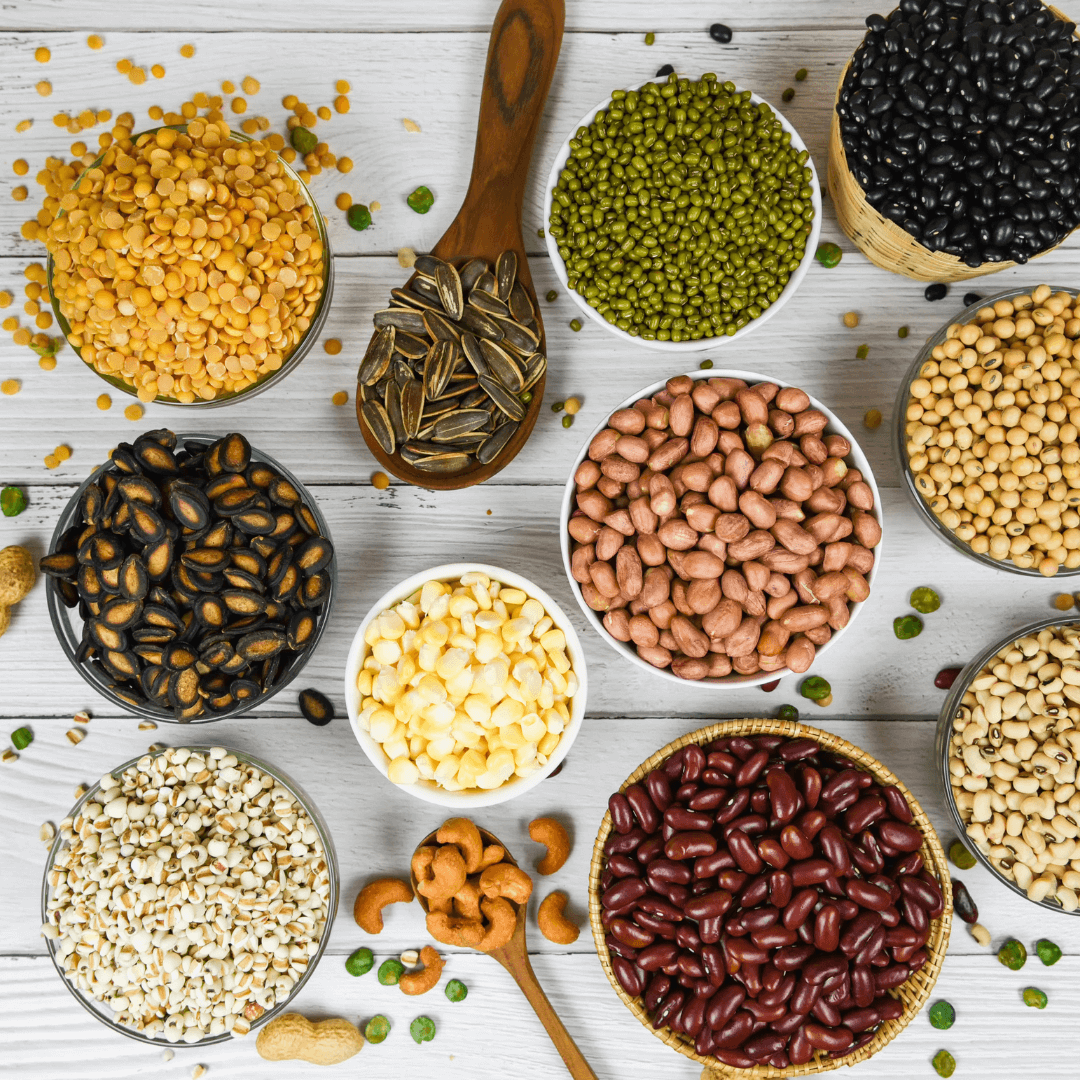
3) Legumes
Legumes—which include lentils and beans—are rich in fiber, protein, and other anti-inflammatory compounds. Due to their inflammation-reducing nature, legumes are recommended for heart-healthy diets, too. Recent research suggests that legumes contain bioactive compounds with antioxidant and anti-inflammatory properties, so they could be used to treat symptoms of arthritis and other inflammatory diseases.
There are literally thousands of types of legumes in the world. But, some of the most common types include chickpeas, black beans, pigeon peas, white beans, soybeans and soy products, mung beans, red lentils, brown lentils, split peas, and more.

4) Fruit
Nature’s candy is rich in anti-inflammatory compounds, including fiber, vitamin C, pectin, polyphenols, and phytochemicals.
While açaí has its superfood reputation, practically all fruit is packed with anti-inflammatory benefits, including apples, cherries, peaches, plums, red grapes, oranges, lemons, and limes. Fresh or frozen fruit is best—many canned fruits contain added sugar.

5) Vegetables
The vegetable world is rich in anti-inflammatory foods. Dark leafy greens like spinach, kale, and collard greens are good sources of fiber, antioxidants, and polyphenols. Broccoli contains sulforaphane, an antioxidant that helps reduce inflammation. Bell peppers contain vitamin C and mushrooms contain compounds called phenols. For an anti-inflammatory meal, you could serve roasted broccoli and tofu scramble made with turmeric over brown rice.
Food is just one factor that could help reduce the symptoms of an autoimmune disorder. Everybody is different, and what works for one person might not benefit someone else. If you are dealing with the symptoms of an autoimmune disease or expect that you may be, it’s best to see your doctor.